Spotlight on the Kolb Lab: Advancing Pulmonary Research with the Compresstome Vibratome
- Original post date:
Share on social
About the Kolb Lab
The Kolb lab, located at the Firestone Institute for Respiratory Health at St. Joseph’s Hospital and the McMaster Immunology Research Centre in Hamilton, Ontario, is spearheaded by Dr. Martin Kolb, a globally recognized authority in pulmonary research (Figure 1). Dr. Kolb’s distinguished career was recently celebrated with his election as a Fellow of the Canadian Academy of Health Sciences (CAHS), a prestigious accolade in Canadian health sciences.
Focused on understanding the biological mechanisms of lung injury, repair, and fibrosis, the Kolb lab is particularly dedicated to unraveling the complexities of idiopathic pulmonary fibrosis (IPF). This fatal interstitial lung disease is marked by progressive lung scarring and declining respiratory function, with no current treatments capable of reversing its course. Addressing these critical challenges, the Kolb lab integrates cutting-edge research methodologies with translational applications to explore novel therapeutic strategies and deepen our understanding of IPF pathogenesis.
The lab fosters a collaborative environment, bringing together undergraduate and graduate students, postdoctoral fellows, and technical experts. Among its standout researchers is Safaa Naiel, a PhD student supported by the prestigious CIHR Canada Graduate Scholarship, whose work focuses on the role of pro-fibrotic macrophages in lung fibrosis.
Macrophages are central to lung fibrosis, contributing both to its progression and resolution. However, their remarkable adaptability within the lung microenvironment makes them difficult to study using traditional in vitro models. The Kolb lab tackles this challenge with innovative experimental approaches to capture the dynamic roles and functional states of macrophages in the fibrotic milieu.
The Role of Precisionary’s Compresstome Vibratome

Central to the Kolb lab’s research is the use of the Compresstome Vibratome, which enables the preparation of precision-cut lung slices (PCLS). This tool has become indispensable for studying lung tissue in a physiologically relevant context, facilitating the investigation of disease mechanisms and therapeutic strategies while providing a dynamic ex vivo model for immune cell behavior in the lung.
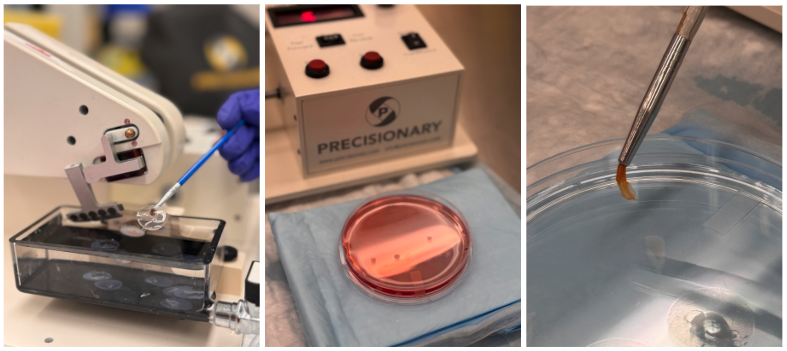
In a recent study published in Biomaterials (impact factor: 15.3), the Kolb lab demonstrated the therapeutic potential of yeast beta-glucan microparticles (PGX-YBG) in modulating macrophage behavior during lung fibrosis. Led by Safaa Naiel (Figure 2), this research highlights the innovative application of the Compresstome Vibratome in generating high-quality PCLS for experimental studies.
Using the Compresstome, the team prepared 500 µm-thick lung slices from mouse lungs, inflated with low-melting-point agarose (Figure 3). These slices were then cultured and exposed to cytokines to induce macrophage polarization into either pro-inflammatory or pro-fibrotic phenotypes. This approach established two models: one representing infiltrating monocytes and another simulating differentiated alveolar and interstitial macrophages.
The study revealed that PGX-YBG treatment effectively shifted macrophages away from a pro-fibrotic phenotype toward an anti-fibrotic state, without compromising lung tissue viability. These findings were substantiated by biomarker analyses and tissue microarray assessments, positioning PGX-YBG as a promising therapeutic strategy for mitigating fibrosis.
Bridging the Gap Between Models
The Kolb lab’s work underscores the critical role of PCLS in bridging the gap between cellular and animal models. The Compresstome Vibratome enables biologically relevant and translational approaches to studying macrophage behavior and their contributions to lung fibrosis, paving the way for innovative therapies and a deeper understanding of IPF.
This spotlight on the Kolb lab showcases how Precisionary Instruments’ Compresstome Vibratome continues to drive advancements in pulmonary research and therapeutic development.
Share on social
